New findings spotlighted during event that examines important science and topics in quality care.
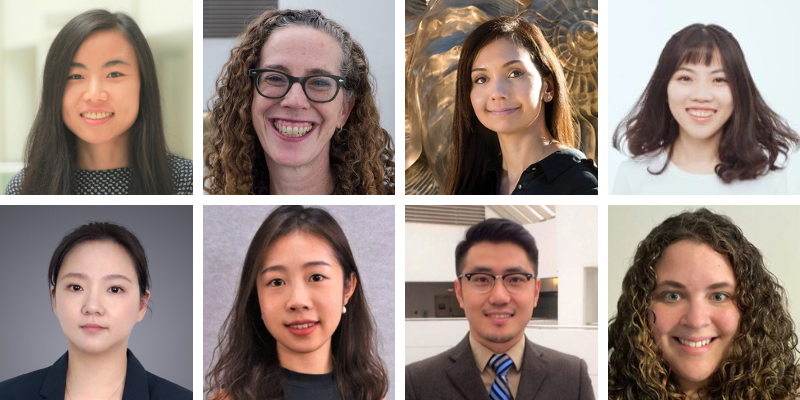
Several ACS findings were presented at the annual American Society of Clinical Oncology (ASCO) Quality Care Symposium in Boston, MA, Oct. 27 – 28. They included the following, pictured above, from top to bottom, left to right:
- A new study, led by Jingxuan Zhao, senior associate scientist, health services research, showed among patients receiving outpatient cancer treatment in two sites (the Mayo Clinic in Phoenix, Arizona and at the University of Mississippi Medical Center in Jackson, Mississippi), most people could understand basic health insurance terms, such as premiums and deductibles. However, the study also showed that relatively high percentages of patients did not understand terms such as provider networks and formularies and had trouble calculating out-of-pocket expenses.
- A new study, led by Dr. Robin Yabroff, scientific vice president, health services research, with researchers at ACS and the National Cancer Institute, shows only about a quarter of individuals newly diagnosed with advanced cancers had documented physician discussions about costs ofcare, which may hinder identifying patient needs and tracking outcomes of referrals for assistance. Growing costs of cancer care can result in financial hardship for patients, and many professional organizations recommend patient-physician discussions about expected treatment costs as part of high-quality care. Documentation of these discussions is critical as even privately insured patients may find care unaffordable without additional assistance.
- New research, led by Dr. Leticia Nogueira, scientific director, health services research, and scientists at ACS and the University of California, San Francisco, shows individuals in the United States undergoing radiotherapy for non-small cell lung cancer (NSCLC) who are exposed to wildfires near the treating facility have worse overall survival than unexposed individuals.
- A new study, led by Kewei Sylvia Shi, associate scientist in health services research, shows that adults in the United States with prior insurance coverage disruptions are significantly less likely to receive guideline-concordant and past-year cancer screening, compared to people with continuous coverage. People without health insurance coverage had the lowest screening levels.
- A new study, led by Qinjin Fan, senior scientist, health services research, found that adults in the United States with stage IV cancer living in nonmetropolitan, socioeconomically deprived areas, the southern U.S., or being treated at community facilities had lower accessibility to palliative care physicians than their counterparts in other areas. Patients who had higher geographic accessibility to palliative care providers were more likely to receive the care in both metropolitan and nonmetropolitan areas.
- A new study, led by Nuo Nova Yang, associate scientist in health services research, found that while the percentage of late-stage diagnoses decreased since 2018 across the United States, patients in states with no or few regulations on short-term limited duration (STLD) insurance sales had a net increase in late-stage cancer diagnoses.
- In two new abstracts, led by Dr. Jason Zheng, senior principal scientist, health services research, crowdfunding campaigns, like GoFundMe, are being used by survivors of cancer in the United States in growing numbers to help pay for medical and other basic household expenses. The use of these campaigns underscores the fragility of financial safety nets for patients and their families.
- A new study, led by Jessica Star, associate scientist, cancer risk factors & screening surveillance research, shows state Medicaid expansion status was associated with higher screening for colorectal and breast cancers and lower socioeconomic insecurity (food and financial) within federally qualified health centers (FQHCs) during the COVID-19 pandemic in the United States from 2020 and 2021.